Cornea Transplant Procedure
14
Mar
2022
What is Cornea Transplant?
A cornea transplant (keratoplasty) is a surgical procedure that involves replacing part of your cornea with corneal tissue from a donor. Your cornea is a transparent, dome-shaped surface of your eye. It is where light enters your eye and is a large part of your eye's ability to see clearly.
A cornea transplant could restore vision, reduce pain, and improve the appearance of a damaged or diseased cornea.
Most cornea transplant procedures are successfully completed. But cornea transplant carries a small risk of complications, like the rejection of the donor cornea.
Why it is done
A cornea transplant is most frequently used to restore vision to a person with a damaged cornea. A cornea transplant could also relieve pain or other signs and symptoms related to cornea diseases.
A number of conditions could be treated with a cornea transplant, including:
- A cornea that bulges outward (keratoconus)
- Fuchs' dystrophy, a hereditary condition
- Thinning or tearing of the cornea
- Cornea scarring, caused by infection or injury
- Swelling of the cornea
- Corneal ulcers not responding to medical treatment
- Complications caused by previous eye surgery
Risks
The cornea transplant is relatively safe. Still, it does carry a small risk of severe complications, such as:
- Eye infection
- Pressure increases within the eyeball (glaucoma)
- Issues with the stitches used to secure the donor cornea
- Rejection of the donor cornea
- Bleeding
- Retinal problems, like retinal detachment or swelling
Signs and symptoms of cornea rejection
Your body's immune system could mistakenly attack the donor cornea. This is known as rejection, and it may require medical treatment or another cornea transplant.
Schedule an urgent appointment with your eye doctor if you notice signs and symptoms of rejection, like:
- Loss of vision
- Eye pain
- Red eyes
- Sensitivity to light
Rejection happens in approximately 10 percent of cornea transplants.
How you prepare
Before cornea transplant surgery, you will undergo:
- A thorough eye examination - Your eye doctor looks for conditions that may cause complications after surgery.
- Measurements of your eye - Your eye doctor determines what size donor cornea you require.
- A review of all medications and supplements you are taking - You might need to stop taking specific medications or supplements before or after your cornea transplant.
- Treatment for other eye problems - Unrelated eye problems, like infection or inflammation, could reduce your chances of a successful cornea transplant. Your eye doctor will treat those problems prior to your surgery.
Finding a donor cornea
The corneas used in cornea transplants come from deceased people. Corneas are not used from people who died from unknown causes or from donors who had specific conditions, like diseases that could spread, previous eye surgery, or eye disease.
Unlike with organs like livers and kidneys, people needing cornea transplants do not require tissue matching. In the United States, donor corneas are widely available so there is usually not a long waiting list.
Procedures to transplant a section of the cornea
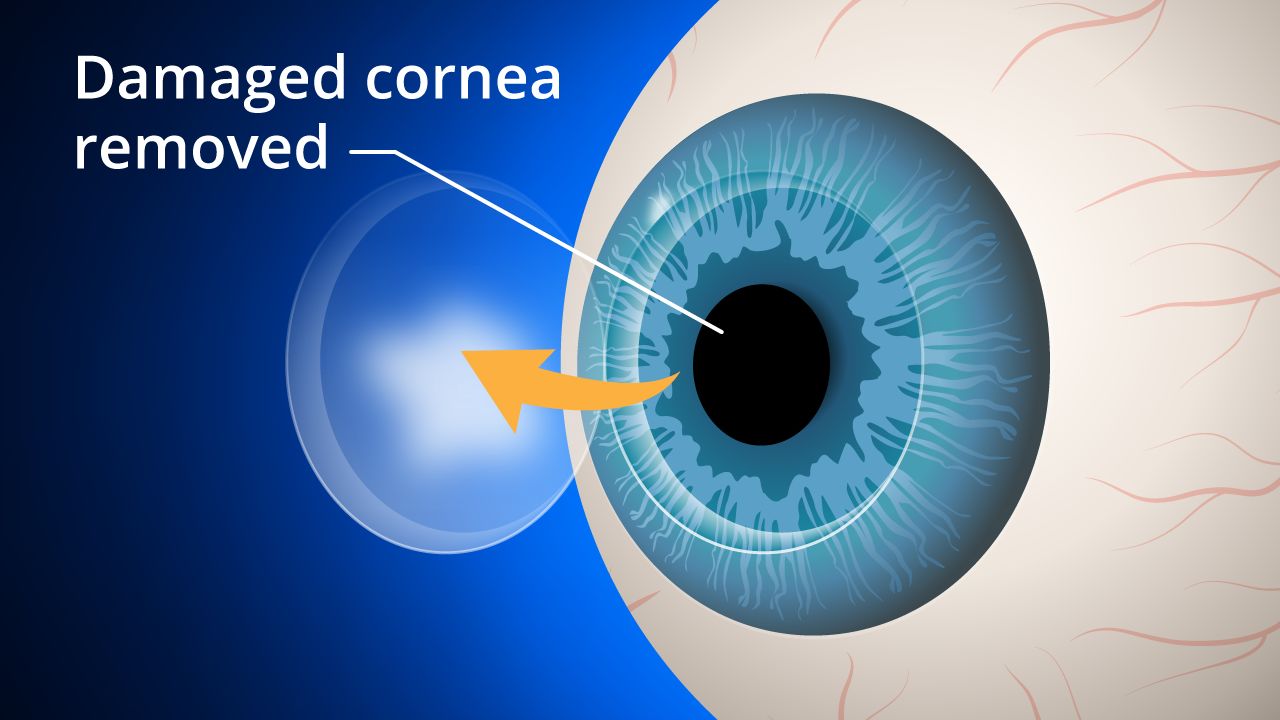
A cornea transplant removes either the complete thickness or partial thickness of the diseased cornea and replaces it with healthy donor tissue. Your cornea surgeon will decide what method should be used. These types of procedures consist of:
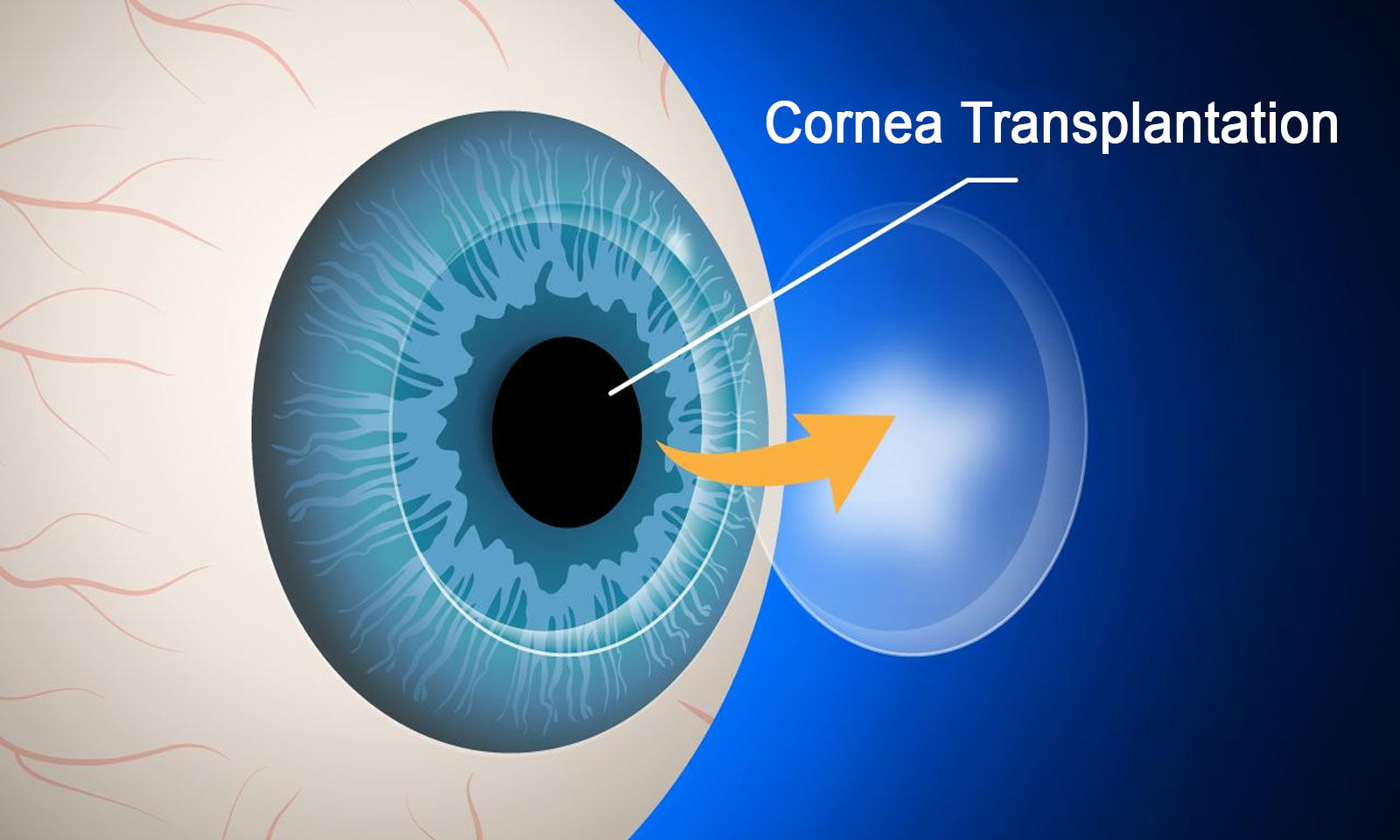
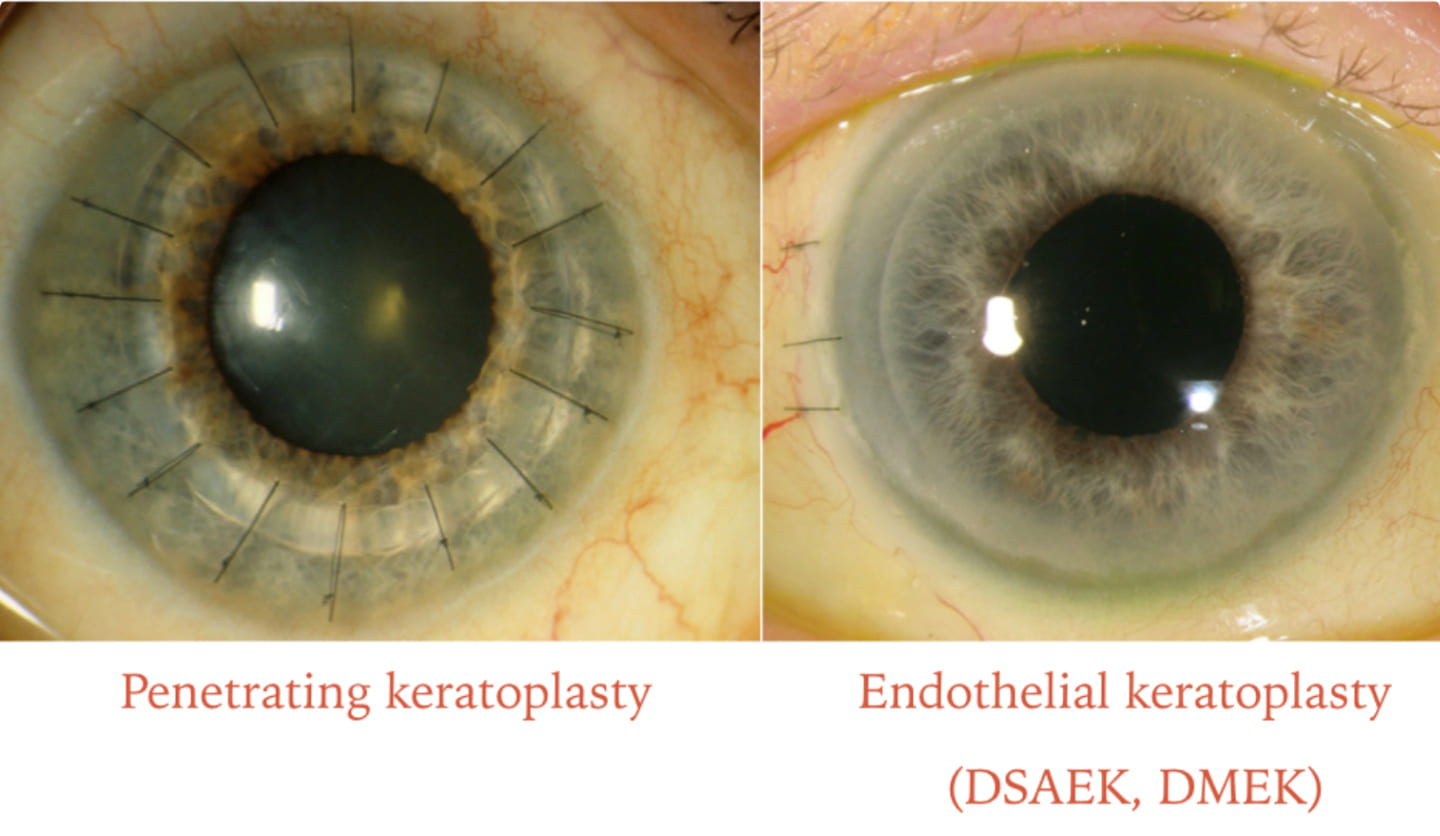
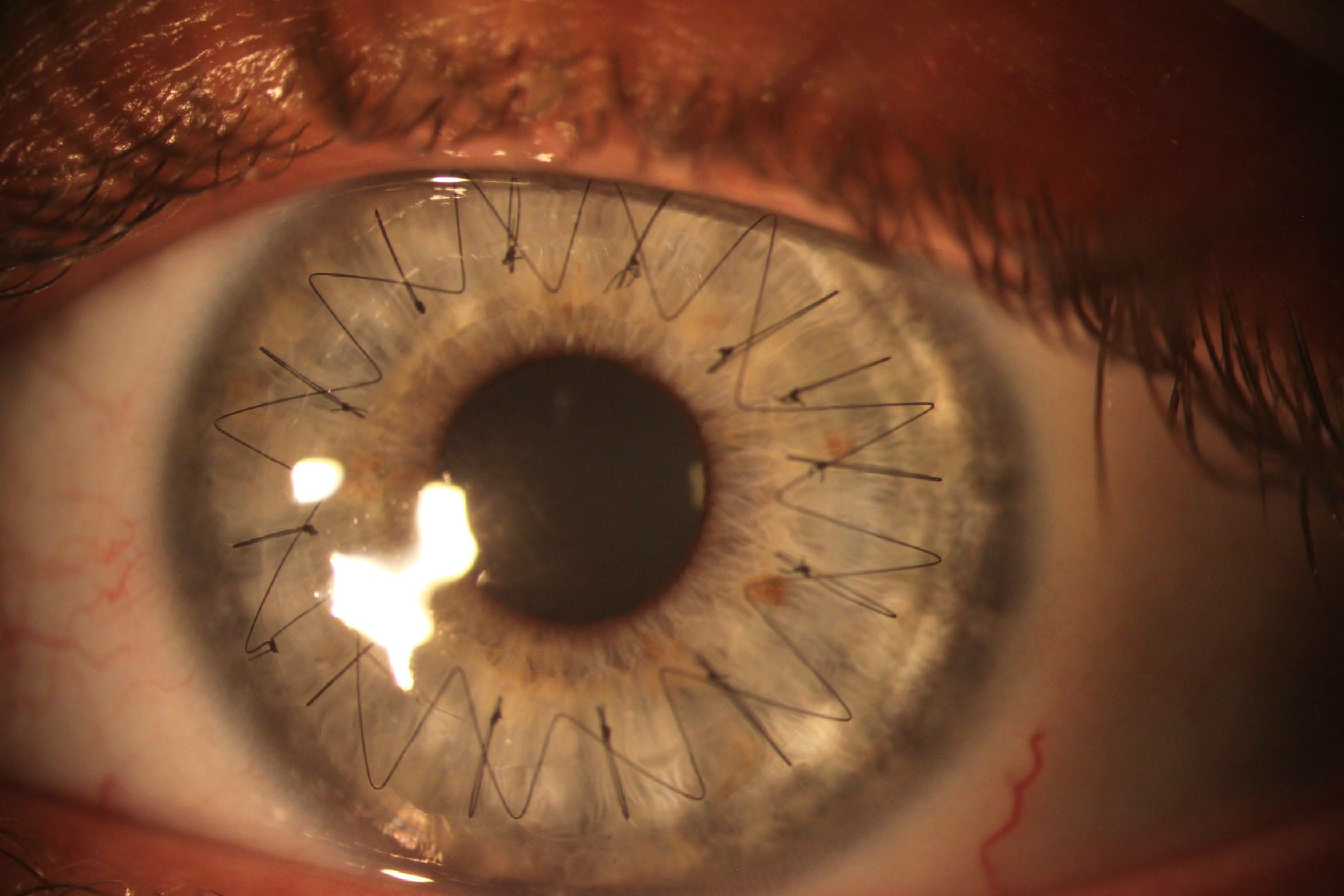
- Penetrating keratoplasty (PK) is a complete-thickness cornea transplant. Your surgeon cuts through the complete thickness of the abnormal or diseased cornea to remove a small button-sized disk of corneal tissue. A special instrument is used to make this exact circular cut.
The donor cornea, cut to fit, is placed into the opening. Your surgeon then uses stitches (sutures) to stitch the new cornea in place. The stitches may be removed at a later visit with your eye doctor. - Endothelial keratoplasty (EK) - These procedures remove diseased tissue from the back corneal layers, including the endothelium and a slim layer of tissue that protects the endothelium from injury and infection (Descemet membrane). Donor tissue is a replacement for removed tissue.
There are 2 types of endothelial keratoplasty. The first type, known as Descemet stripping endothelial keratoplasty (DSEK), uses donor tissue to replace about one-third of the cornea.
The second type, known as Descemet membrane endothelial keratoplasty (DMEK), uses a much thinner layer of donor tissue. The tissue used in DMEK is extremely thin and delicate. This procedure is more difficult than DSEK and is commonly used. - Anterior lamellar keratoplasty (ALK) - Two different methods remove diseased tissue from the front corneal layers, involving the epithelium and the stroma, but leave the back endothelial layer in place.
The depth of cornea damage determines the type of ALK procedure that is right for you. Superficial anterior lamellar keratoplasty (SALK) only replaces the anterior layers of your cornea, leaving the healthy stroma and endothelium intact. A deep anterior lamellar transplant (DALK) procedure is used when cornea damage extends further into the stroma. Healthy tissue from a donor is then connected (grafted) to replace the removed portion. - Artificial cornea transplant (keratoprosthesis) - In some cases, if people are not eligible for a cornea transplant from a donor cornea, they may receive an artificial cornea (keratoprosthesis).
Your doctor will discuss which method of corneal transplant surgery is the best one for you, what to expect during the procedure, and explain the risks of the procedure.
What you can expect
During the procedure
On the day of your cornea transplant, you will either be given a sedative to help you relax and a local anesthetic to numb your eye, or you will be put to sleep. No matter what, you should not feel pain.
The surgery is done on one eye at a time. The amount of time spent in surgery is different and depends upon your situation.
After the procedure
Once your cornea transplant is completed, you could expect to:
- Receive medications - Eyedrops and, at times, oral medications immediately after cornea transplant and during recovery will help control infection, swelling, and pain. Eyedrops to suppress the immune system help in preventing cornea rejections.
- Wear eye protection - Eyeshields or glasses protect your eye as it recovers.
- Lie on your back - Depending on the type of transplant, you may have to do this for a while after surgery to help the new tissue stay in place.
- Avoid injury - Plan to take it easy after your cornea transplant, and gradually work your way up to your normal activities, including exercise. Do not rub or squeeze your eye. For the rest of your life, you will need to take extra precautions to avoid harming your eye!
Results
Most people who receive a cornea transplant will have their vision at least partly restored. What you could expect after your cornea transplant depends on the reason for your surgery and your health.
Your risk of complications and cornea rejection persists for years after your cornea transplant. For this reason, consult your eye doctor annually. Cornea rejection could often be managed with medications.
Vision correction after surgery
Your vision may initially be worse than prior to your surgery as your eye adjusts to the new cornea. It could take several months for your vision to improve.
Once the outer layer of your cornea has healed — several weeks to several months after surgery — your eye doctor will work to make adjustments that could improve your vision, such as:
- Correcting unevenness in your cornea (astigmatism) - The stitches that keep the donor cornea in place on your eye may cause dips and bumps in your cornea, making your vision blurry in spots. Your doctor may correct some of this by releasing some stitches and tightening others.
- Correcting vision problems - Refractive errors, like near-sightedness and farsightedness, could be corrected with glasses, contact lenses, or, in some cases, laser eye surgery.
Hill Regional (HRH) Hospital is here to assist all your medical needs with specialists and surgeons trained and experienced in the most advanced treatments. Our highly qualified doctors, nurses, and administrators are dedicated to caring for you with compassion in our state-of-the-art facilities.
Call us on 254-580-8500 to book an appointment with our specialist doctors.